
Nano cancer drugs move to the next level: humans
By Eric Smalley, Technology Research NewsMaking cancer drugs safe and effective enough for humans increasingly comes down to packaging. A growing number of cancer therapies packaged in infinitesimal particles are making their way to patients.
 |
The lung cancer patients received a therapeutic gene that reprogrammed many of their cancer cells to die of old age like healthy cells. The gene was packaged in fatty spheres measuring 100 to 200 nanometers in diameter, 25 to 50 times smaller than a red blood cell.
"The difficulty we have with most therapies is in delivery: getting enough of it to the tumor cell," said Jack A. Roth, director of the W. M. Keck Center for Innovative Cancer Therapies at M. D. Anderson. "There's the problem of resistance to the therapy as well. I think nanoparticles potentially could overcome both of these issues."
Biopsies from the lung cancer patients showed that the nanoparticles did indeed deliver. Tumor cells took up about 10 times more of the particles than healthy cells, and the inserted gene functioned in the cancer cells, Roth said. This initial study is too small, however, to prove that the gene therapy was directly responsible for doubling the patients' survival time.
The study also showed that patients can tolerate relatively high doses of substances delivered this way, said Roth. "We've undergone about a sixfold escalation in the dose and we still have not reached a maximum tolerated dose," he said.
The right kind of toxic
Finding the right dose is one of the most important aspects of cancer research because cancer treatments are designed to attack cells, and the difference between an effective dose and a dose with unacceptably high side effects can be uncomfortably small. Cancer drugs work in a number of ways, including triggering natural cell death, shutting down blood vessel formation in tumors, making cancer cells more susceptible to other chemotherapy drugs and radiation, and recruiting the immune system to attack cancer cells.
The initial clinical trials of experimental cancer therapies have confirmed researchers' expectations that nanoparticles greatly reduce the toxicity of anticancer agents and significantly extend the time the drugs circulate in the body. Lower toxicity means fewer side effects like a weakened immune system, nausea, fatigue and organ damage. Longer circulation times allow more of the drug to reach its target.
This means that, in addition to improving the performance of existing cancer drugs, nanoparticle-based drug delivery techniques could expand the number and type of drugs used to treat cancer. "We may be able to deliver drugs which now we're really not able to deliver because they're very unstable, they're not soluble enough, enough of the drug doesn't reach the tumor, they're too toxic," Roth said.
It may also allow oncologists to prescribe treatments when they ordinarily wouldn't take the risk. Physicians often pick up indicators of cancer, for example detecting elevated levels of proteins associated with cancer in blood tests, but subsequent medical imaging fails to find tumors, said Mark E. Davis, a chemical engineering professor at the California Institute of Technology and developer of nanoparticle cancer treatments.
"If we could create these new, very selective therapies with essentially minimal side effects, that would open up the possibility of treating people in even a prophylactic sense," said Prof. Davis.
The low toxicity of nanoparticle-packaged chemotherapy drugs also makes it easier for oncologists to prescribe drugs in combination, said Prof. Davis. Ordinarily, "when you try to build combination therapies, what you're doing is just piling on side effect A to side effect B to side effect C," he said.
Smaller and smarter
The nanoparticle-based cancer therapies in or entering human cancer studies are the leading edge of a wave of sophisticated drugs emerging from university spinoffs and startups. Within the next year, companies will petition the FDA for approval to start human trials for at least three more nanoparticle-based anticancer therapies, according to Piotr Grodzinski, director of the National Cancer Institute's Alliance for Nanotechnology in Cancer.
The nanoparticle drug delivery therapies moving through the regulatory process are descendents of the drug Doxil, a nanoparticle-encapsulated form of the established cancer drug doxorubicin. Doxil, now used to treat ovarian cancer and multiple myeloma, received FDA approval in 1995 for treating Kaposi's sarcoma in people with AIDS. Several similar nanoparticle cancer therapies have reached the market in the last few years.
These first-generation nanoparticle therapies are microscopic balloons filled with standard chemotherapy drugs. The second-generation nanoparticle drug delivery systems in or entering human trials are more sophisticated.
They can carry genetic material as well as traditional small-molecule drugs. Some of the nanoparticles are smaller still, which makes them more effective at traversing the bloodstream and entering cells. Some sport molecules that let them selectively bind to and penetrate cancer cells, then quickly dump their payloads once inside.
And some nanoparticles carry no drugs at all; the nanoparticles themselves are the therapeutic agent. The particles accumulate in or near tumor cells. Focusing a magnetic field, radio waves or infrared light on the tumor heats the particles enough to kill the cells.
Rice University spinoff Nanospectra Biosciences has received FDA approval to begin a pilot study of 15 patients to test gold-covered glass nanoparticles. The nanoparticles accumulate in tumors and heat up when exposed to infrared light, killing the surrounding tumor cells.
Some proposed therapies based on the heat-to-kill technique have raised safety concerns because they use carbon nanotubes or metal nanoparticles that haven't been tested in humans. Animal studies have found that unmodified carbon nanotubes can accumulate in organs. Many of the drug delivery nanoparticles in or near human trials, however, are made from FDA-approved lipids or polymers.
Clinical trials
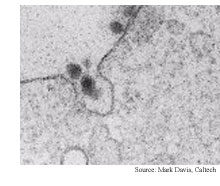
Insert Therapeutics, a Caltech spinoff that merged with another Caltech spinoff, Calando Pharmaceuticals, in February, is conducting a small clinical study of its 40-nanometer polymer-based nanoparticle carrying the anticancer compound camptothecin. The patients in the study have advanced solid tumor cancers. "We have very low toxicity, and we have circulation times in humans that are several days," said Prof. Davis, who founded Insert Therapeutics and Calando.
The 20 patients in the trial have had a fairly high quality of life while on the treatment, said Prof. Davis. "Our poster child for this trial is a gentleman who had metastatic pancreatic cancer and he's now still stable after 22 months."
The company has filed for FDA approval to begin a study of 150 patients in the US and Eastern Europe and plans to begin treating patients by the third quarter of this year.
Calando is weeks away from treating the first patient with a nanoparticle that carries short interfering RNA molecules (siRNA), Prof. Davis said. RNA interference, the subject of the 2006 Nobel Prize in medicine, shuts off specific genes, but the siRNA needs to be delivered directly to tumor cells to be effective.
SiRNA therapies could be especially helpful for treating patients who develop resistance to traditional chemotherapy. "Drug resistance often occurs when cells take advantage of mechanisms for ridding themselves of small molecules," said Ian McLachlan, chief scientific officer of Protiva Biotherapeutics, a Canadian biotechnology company. Those mechanisms generally don't exist for removing larger biological molecules like DNA and RNA, he said.
Protiva is wrapping up a 15-patient trial of a nanoparticle-delivered gene therapy for melanoma. The study encountered adverse effects that will require the company to redesign the nanoparticle, McLachlan said. The company is planning to start a trial towards the end of the year of a smaller nanoparticle designed to deliver siRNA, McLachlan said.
The number of nanoparticle cancer drugs entering human trials is on the rise because researchers are gaining experience in designing drug delivery nanoparticles. A Massachusetts Institute of Technology research team has developed a library of 1,200 lipid nanoparticles, opening the way for researchers to choose a nanoparticle based on the properties needed for delivering a particular drug to treat a specific disease rather than build a nanoparticle from scratch.
Cancer research periodically takes major steps forward: combination therapy in the 1960s, improved imaging technologies in the 80s and 90s, and monoclonal antibodies in the last decade. Ten years from now nanoparticle drug delivery systems could be viewed in the same light. "I think it's going to change the way we deliver drugs," Roth said.
Advertisements:
April 18, 2008
Features:
View from the High Ground Q&A
How It Works
RSS Feeds:
News
Ad links:
Buy an ad link
| Advertisements:
|
 |
Ad links: Clear History
Buy an ad link
|
TRN
Newswire and Headline Feeds for Web sites
|
© Copyright Technology Research News, LLC 2000-2006. All rights reserved.